Understanding Plantar Fasciitis and High Arches
While plantar fasciitis is often associated with flat feet, people with high arches are equally susceptible to plantar fasciitis. The plantar fascia – a thick band of tissue running along the bottom of your foot – acts as a shock absorber and supports the foot’s arch with every step.
Individuals with high arches typically have a rigid foot that absorbs shock poorly, causing impact to be transferred up through the heel and fascia. Over time, this constant tension can lead to plantar fasciitis and its symptoms, such as stabbing pain in the heel or arch, especially in the morning. This stabbing pain is often sharp and intense with the first few steps of the day, then may diminish as you move around. If left untreated, the strain can extend up the kinetic chain, causing discomfort in the ankles, knees, or even the lower back. That’s why it’s important to manage your plantar fasciitis and seek help from a podiatrist before the issue worsens.

Why High Arches Cause Plantar Fasciitis
If the foot has a high arch, most of the load falls on the heel and ball of the foot rather than being evenly distributed across the sole. This imbalance increases stress on the plantar fascia, which connects the heel bone (calcaneus) to the toes.
High-arched feet are also more prone to ankle instability and ankle sprains due to structural imbalance and are at greater risk of injury. Runners, dancers, factory workers, and individuals who stand for extended periods are particularly vulnerable.
High arches without adequate cushioning or arch support are a recipe for chronic heel pain. External factors, such as worn-out shoes, thin soles, or walking barefoot on hard floors, which are common habits in Singapore’s warm climate, can also aggravate the problem.

What Does It Feel Like?
For many, the first sign of plantar fasciitis due to a high arch is a sharp or stabbing pain under the heel of the affected foot when getting out of bed in the morning. As the day progresses, the discomfort may ease slightly but often returns after prolonged standing or walking. Some people describe a tightness that extends along the sole of the affected foot. Others experience swelling or tenderness near the heel.
If the pain becomes persistent or begins affecting both feet, it’s essential to seek professional assessment. Ignoring symptoms can lead to compensatory changes in your gait, worsening the condition and potentially triggering secondary issues such as Achilles tendonitis or metatarsalgia.

Diagnosing Plantar Fasciitis in High Arches
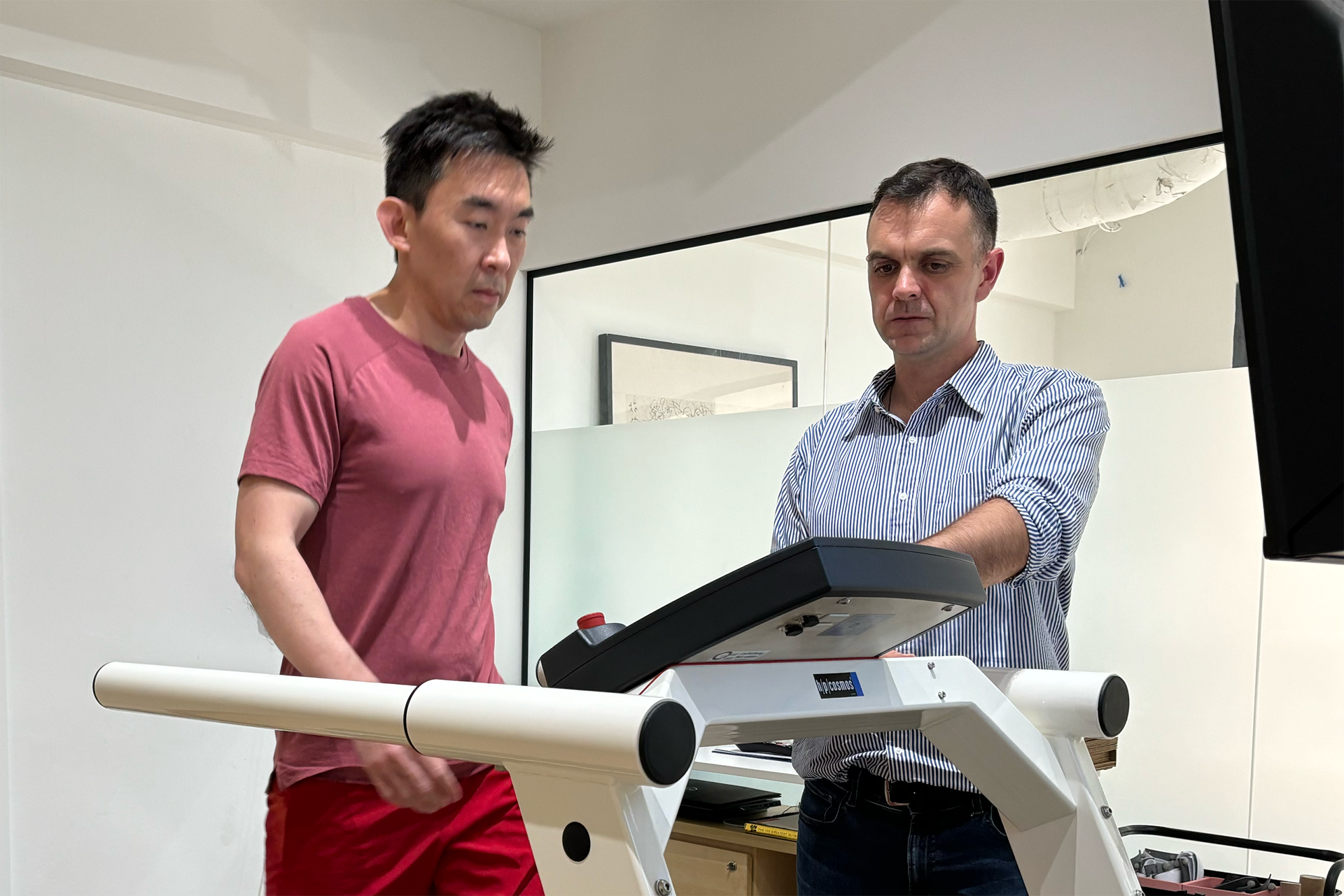
A thorough assessment is the first step toward recovery. During your visit to The Foot Practice, the podiatry team will evaluate your foot structure, muscle strength and walking mechanics, starting with a physical exam. Using the RehaWalk® pressure-sensor treadmill, your gait pattern and pressure points are mapped in real time. This data reveals how your arches move under load and will highlight the specific areas of excessive strain.
A detailed footwear assessment follows, reviewing how your current shoes support or stress your arches. In some cases, imaging tests such as ultrasound or X-ray may be used to confirm inflammation, rule out heel spurs, or assess soft-tissue integrity. This comprehensive approach ensures that the root biomechanical cause is identified rather than just managing symptoms. Consulting our expert podiatrist is important for accurate diagnosis and management.
At home, you can try the ‘wet feet’ test to help identify high arches. Simply wet the soles of your feet and stand on a piece of paper. Examine the imprint left behind. If you see only a narrow band or almost no imprint where your arch should be, this may indicate high arches. This, however, cannot diagnose plantar fasciitis or determine the severity of your high arches, but it can help you understand your situation before you visit a specialist.

Managing Pain and Discomfort
To reduce pain and inflammation, it’s important to address both the symptoms and the root causes of your pain. Resting the affected foot and avoiding overusing it can help prevent further injury. Applying ice to the heel and bottom of your foot can reduce inflammation and provide temporary relief from plantar fasciitis pain. Supportive shoes with built-in arch support, custom orthotics, and night splints are all effective in reducing pressure on the plantar fascia and alleviating heel pain.
Physical therapy is another cornerstone of managing plantar fasciitis discomfort. A qualified podiatry team may recommend stretching exercises to improve flexibility in the calf muscles and plantar fascia, as well as plantar fascial release techniques to ease tension. These exercises not only reduce pain but also help prevent future flare-ups by strengthening the foot’s arch and improving overall foot mechanics.
Advanced therapies, like Shockwave Therapy, can stimulate blood flow and promote healing in stubborn cases. Surgery is rarely needed, but may be considered if conservative treatments fail to provide relief after several months.
Maintaining good foot health is key to preventing plantar fasciitis from returning. Choose supportive shoes, avoid walking barefoot on hard surfaces, and take regular breaks to rest and stretch, especially if your lifestyle or job puts you at higher risk.

The Role of Orthoses in Management
Custom orthotics are a personalised solution that can provide targeted support for the arch, tailored to your unique foot structure. These specialised insoles are designed to support the natural curvature of your foot, redistribute weight, and reduce excessive tension on the fascia.
At The Foot Practice, custom orthoses for women’s shoes are crafted to fit comfortably within high heels or dress shoes without compromising style. For others, functional orthoses can be tailored to everyday footwear, sports shoes, or work boots.
By restoring balance to the foot, these inserts help prevent overloading of the heel and forefoot while improving overall stability. They’re particularly effective for those seeking the best insoles for high arches and plantar fasciitis, offering precision support that off-the-shelf products often fail to deliver.

Complementary Therapies and Rehabilitation
A structured rehabilitation plan can significantly accelerate recovery and prevent recurrence of plantar fasciitis. In addition to mobilisation exercises, physical therapy is often recommended as part of the rehabilitation process to help rebalance and stabilise the foot.
Mobilisation exercises are used to restore joint flexibility, particularly through the ankle and midfoot, reducing strain on the fascia. Your podiatrist may also prescribe targeted stretching exercises, including calf stretches to release tightness in the calf muscles, which often contribute to heel pain. Night splints are another conservative treatment that helps stretch the plantar fascia and calf muscles overnight, alleviating symptoms and preventing worsening.
For chronic or stubborn cases, Shockwave Therapy is another effective, non-invasive treatment. By delivering focused acoustic pulses to the affected area, this therapy stimulates blood flow and cellular regeneration, encouraging natural healing. It’s handy for patients with long-standing pain who haven’t responded to conservative care.
Incorporating technology like RehaWalk gait analysis into rehabilitation helps track improvements in movement patterns, ensuring the fascia isn’t continually overstressed as healing progresses.

Choosing the Right Footwear
Finding high arch shoes for plantar fasciitis is an essential part of recovery and prevention. Shoes should provide adequate arch support, cushioning, and a slightly raised heel to reduce stress on the fascia. A firm heel counter adds stability, while flexible midsoles allow for natural movement without excessive strain.
Many stylish footwear brands now offer designs that incorporate podiatric principles, making it easier to find options that are both fashionable and functional. Pairing these shoes with custom orthoses ensures consistent support whether you’re at work, exercising, or walking around Singapore’s busy streets.
Replacing worn-out footwear regularly is equally important, as old soles and compressed midsoles lose their ability to absorb shock, which can contribute to recurring heel pain.

How Long Does Recovery Take?
Most patients notice improvement within several weeks when following a tailored podiatric plan. For chronic cases or those with longstanding biomechanical imbalances, full recovery may take several months.
However, with the right combination of therapies, including custom orthoses, stretching, Shockwave Therapy, and gait retraining, many patients regain comfort and function far sooner.

Preventing Future Heel Pain
Once symptoms have eased, prevention becomes the priority. Continuing prescribed stretching and strengthening exercises helps maintain flexibility and resilience in the fascia.
Routine podiatric check-ups are invaluable, especially for individuals with naturally high arches, as early intervention can prevent small discomforts from progressing into painful conditions. Maintaining a healthy body weight, incorporating low-impact activities such as swimming or cycling, and avoiding sudden changes in training intensity are practical steps toward sustained foot health.

A Comprehensive Approach to Foot Health
At The Foot Practice, management of plantar fasciitis and high-arch conditions isn’t a one-size-fits-all approach. Every care plan begins with a detailed assessment that blends clinical insight with advanced technology to uncover the specific causes of pain. From custom orthoses that perfectly contour your foot to targeted therapies such as Shockwave Therapy and mobilisation exercises, each intervention is designed to restore movement and comfort. We offer a range of interventions for plantar fasciitis and high arches, including physical therapy, footwear modifications, and orthotic devices.
If you’re struggling with persistent heel pain and suspect it’s linked to high arches, professional podiatric care can make all the difference. Recognising that plantar fasciitis resulting from a high arch is a biomechanical issue rather than just inflammation enables targeted, effective management.
Whether you’re searching for the best insoles for high arches, plantar fasciitis or advice on high arch shoes for plantar fasciitis, our experienced podiatrists can guide you toward lasting relief.
Book a consultation at The Foot Practice today to restore comfort, improve mobility, and prevent future heel pain.