Morton’s neuroma is a painful foot condition that affects thousands of people worldwide, making daily activities a challenge. Discover everything you need to know about Morton’s neuroma, from understanding the condition to treatment options that will get you back to comfort and mobility.
What Is Morton’s Neuroma?
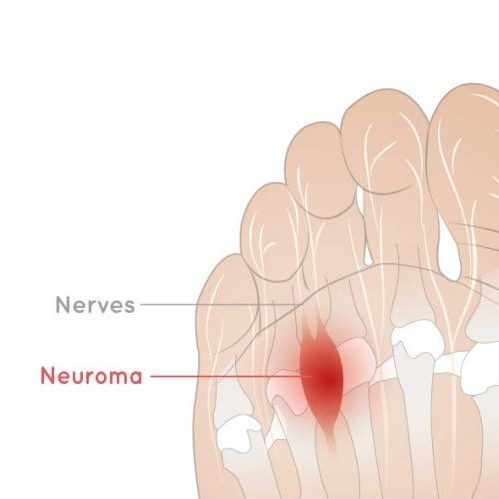
Morton’s neuroma is caused by excess pressure on the nerves of your foot, usually from wearing shoes that are too tight. A small ball of nerve bundles forms a benign tumour on the ball of the foot, usually in the web space between the third and fourth toes. You can’t see it physically, but it’s painful, like you’re standing on a rock.
This condition involves the thickening of tissue around one of the nerves leading to your toes, creating a benign growth that can be very uncomfortable. Morton’s neuroma most commonly occurs between the 3rd and 4th toes, but can also occur between other toes. It’s named after Dr. Thomas George Morton, who first described it in 1876.
The pain of Morton’s neuroma is sharp in the area of the neuroma, but you can also feel burning pain near the ball of your foot. Your toes may also feel numb or experience a burning sensation. Understanding these symptoms is key to early detection and treatment of Morton’s neuroma.
Morton’s Neuroma Symptoms and Signs
There are no visible signs of the neuroma, which is a disorganised non-cancerous growth of nerve cells at the site of a nerve injury. The diagnosis is based on the type and quality of pain you’re experiencing. As mentioned, it may feel like a small rock in your shoe with burning in the ball of the foot that travels to your toes. Your toes may be numb or tingly because the nerve is affected.
Common symptoms of Morton’s neuroma include:
- Sharp, burning pain: The most common symptom of Morton’s neuroma is sharp, burning, or stinging pain in the ball of the foot that may radiate to the toes.
- Sensation of standing on an object: Many patients describe feeling as though they’re standing on a pebble, marble, or a fold in their sock, even when their shoes are empty.
- Numbness and tingling: Due to nerve compression, the affected toes may feel numb, tingly, or as if they are on pins and needles.
- Pain that worsens with activity: Symptoms worsen with weight-bearing activities, such as walking, running, or standing for long periods.
- Relief when removing shoes: Many people with Morton’s neuroma get immediate relief when they remove their shoes and massage their feet.
Pain that varies with footwear: Tight shoes, high heels or shoes with narrow toe boxes worsen symptoms, while wider, more supportive shoes provide relief.

Causes and Risk Factors of Morton’s Neuroma
Morton’s neuroma symptoms start gradually and may be mild and intermittent at first. However, without treatment, the condition worsens over time. What begins as an occasional discomfort can progress to constant pain that affects your mobility and quality of life.
Women experience Morton’s neuroma more often than men because of wearing high heels that put pressure on the nerves going to the toes. They may also wear shoes that are too tight, which can cause pinching of the nerves.
Understanding all the contributing factors can help prevent and treat Morton’s neuroma.
Primary Causes:
- Footwear choices: High-heeled shoes and tight-fitting footwear are the leading causes of Morton’s neuroma. Shoes that compress the toes or have narrow toe boxes create excessive pressure on the forefoot nerves.
- Repetitive stress: You can also develop Morton’s neuroma foot condition if you jog or run repeatedly and strike your foot against the pavement. Any sport that involves tight-fitting shoes, such as rock climbing or skiing, can also put extra pressure on the nerves.
- Foot structure abnormalities: Individuals with foot problems, such as hammertoes, bunions, flat feet, or high arches, are at a greater risk of developing Morton’s neuroma. These conditions alter the normal mechanics of the foot, increasing pressure on specific areas of the foot.
Additional Risk Factors:
- Age and gender: Morton’s neuroma is most common in middle-aged women, particularly those between 40 and 60 years old.
- Occupational factors: Jobs that require prolonged standing or walking, especially in inappropriate footwear, increase the risk of developing Morton’s neuroma.
- Previous foot injuries: Trauma to the foot can lead to scar tissue formation and nerve irritation, which can contribute to the development of Morton’s neuroma.
Genetic predisposition: Some people may have inherited foot structures that make them more prone to nerve compression and Morton’s neuroma.

Diagnosing Morton’s Neuroma
Diagnosing Morton’s neuroma requires a thorough evaluation by a qualified healthcare professional. The diagnostic process involves multiple steps to ensure accurate identification and rule out other potential conditions.
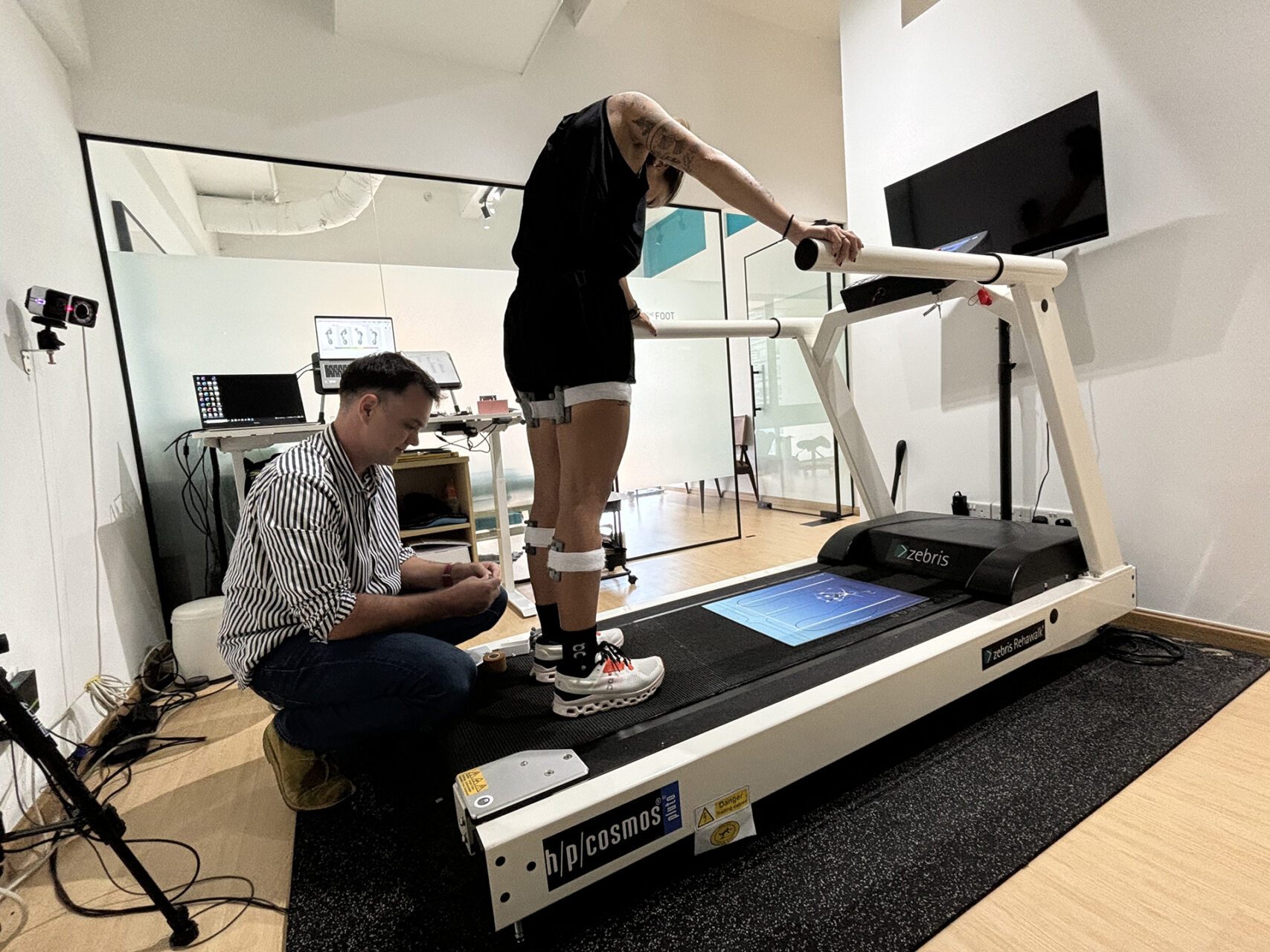
The diagnosis can be made clinically by feeling your foot and looking for a lump or tender area. Sometimes, the podiatrist will use the back of a pencil to gently push the tissue between the toes, feeling for areas of tenderness. During the physical examination, your podiatrist will also perform several specific tests, including Mulder’s, pressure and range of motion assessments.
Diagnostic imaging, including X-rays, ultrasound and MRI scans, can be used to diagnose the condition. X-rays are mainly used to rule out other conditions, such as a stress fracture of one of your metatarsal bones. Ultrasound can be used on the foot to highlight the actual neuroma within the tissues. MRI scans are also effective for diagnosing soft tissue problems. It utilises a strong magnet and radio waves to produce two- and three-dimensional images of the foot. This is an expensive test, so it’s not used often to diagnose Morton’s neuroma. More often than not, a physical examination is all that is necessary.
Diagnosing Morton’s neuroma also involves ruling out other conditions that can cause similar symptoms, such as metatarsalgia (general pain in the ball of the foot), stress fractures, arthritis, plantar plate tears, and intermetatarsal bursitis.
Conservative Morton’s Neuroma Podiatric Interventions
Morton’s neuroma interventions vary depending on how severe your symptoms are and how long you’ve had them. A systematic approach typically yields the best results, starting with conservative treatments and progressing to more aggressive interventions as needed.
- Footwear modifications: The first line for management of Morton’s neuroma is to change your shoe choices. You will be asked not to wear high heels and should wear shoes that give your feet plenty of room. Shoes with wide toe boxes, low heels and adequate arch support can reduce pressure on the affected nerve.
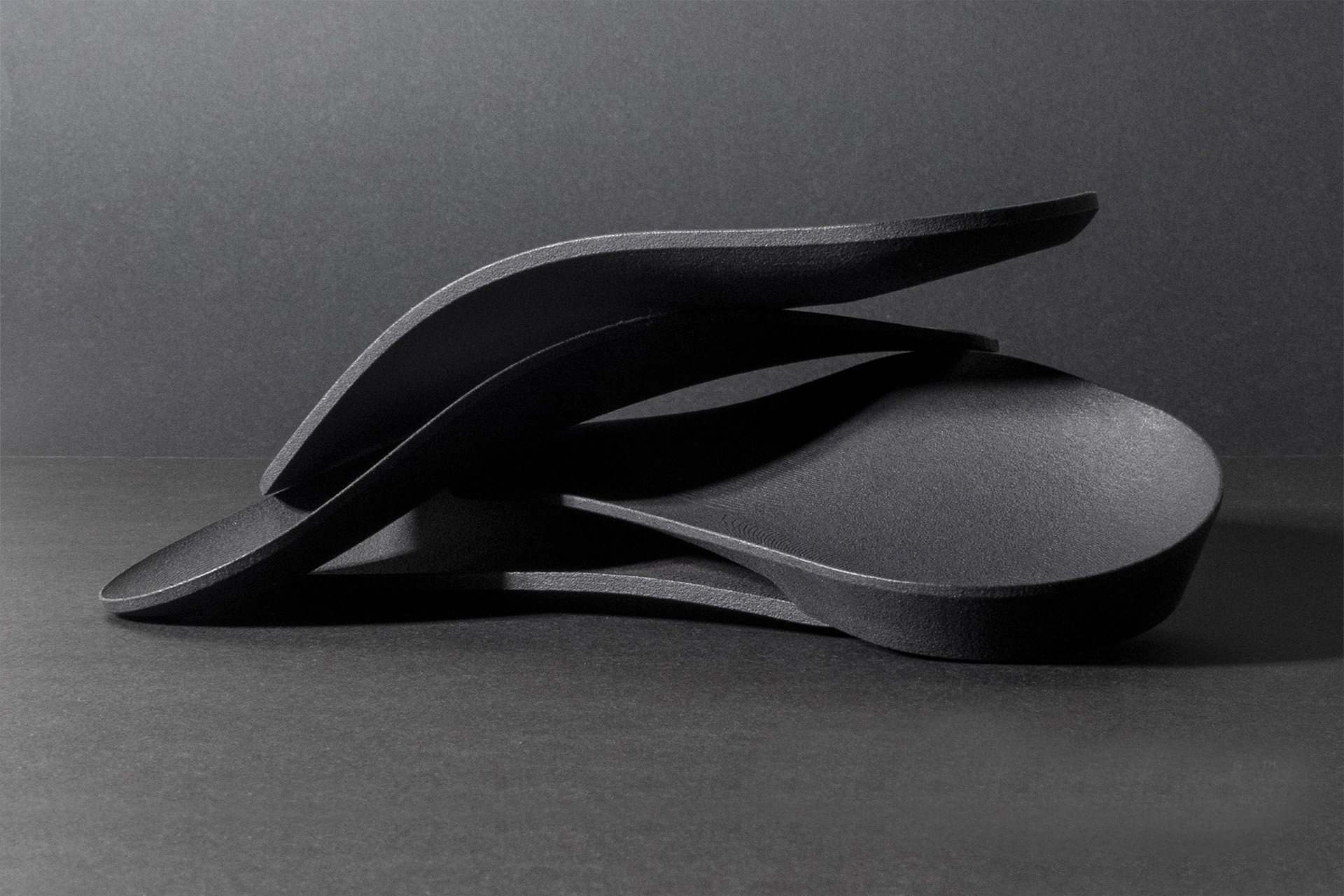
- Morton’s neuroma insoles and orthoses: Our podiatrist may prescribe arch supports or pads to wear inside the shoe to relieve pressure on the nerve. Morton’s neuroma insoles are designed to redistribute pressure away from the affected area and cushion the ball of the foot. Custom-made foot moulds may also be made to support the foot and reduce pain.
- Activity modification: Reducing high-impact activities can help reduce inflammation and facilitate healing.
- Anti-inflammatory medications: Over-the-counter NSAIDs (non-steroidal anti-inflammatory drugs) can help with pain and swelling associated with Morton’s neuroma.
Advanced Treatment & Surgical Options
If conservative podiatric interventions are not effective, our podiatrist may refer you to a doctor who can inject the neuroma with corticosteroids to relieve the inflammation around the nerve bundle. These injections can provide significant pain relief for several months and can be repeated as needed.
Some practitioners use alcohol injections to deaden the nerve and reduce pain. This treatment requires multiple sessions but can provide long-term relief.
When conservative treatments don’t work, surgical intervention may be necessary. If necessary, you may be referred for a surgical procedure to remove tissue that is putting pressure on the neuroma. This spreads out the bones and keeps them from pressing on the neuroma. In severe cases, the neuroma can be cut out. This will relieve the pain, but because it involves cutting the nerve, there can be permanent numbness in the toes.
Surgical options include:
- Neurectomy: Complete removal of the affected nerve portion eliminates pain but results in permanent numbness in the affected toes.
- Decompression surgery: Release of structures compressing the nerve, potentially preserving nerve function while relieving pressure.
Metatarsal surgery: In some cases, shortening or repositioning of metatarsal bones can reduce pressure on the nerve.

Prevention and Long-term Management
Preventing Morton’s neuroma recurrence and managing the condition long-term requires ongoing attention to foot health and lifestyle changes.
Choose shoes with plenty of toe room, good arch support and appropriate heel height for your activities.
To prevent recurrence, continue to use Morton’s neuroma insoles even after symptoms have gone. Regular stretching and strengthening exercises maintain foot flexibility and strength. Being at a healthy weight also reduces pressure on the feet and can prevent Morton’s neuroma from developing.
Regular check-ups with your podiatrist are essential for monitoring your condition and adjusting treatment as needed. Early intervention at the first sign of recurrence can prevent it from worsening.

When to Make an Appointment at The Foot Practice
If you experience pain in your shoes, you may be suffering from Morton’s neuroma or another musculoskeletal condition. Seek immediate attention if you have pain that doesn’t improve with rest, numbness in your toes, pain that affects your daily activities, or symptoms that worsen despite conservative management.
Understanding Morton’s neuroma, recognising the symptoms early, and seeking treatment can help you live an active, comfortable life. Relief is possible through conservative measures, such as Morton’s neuroma insoles, shoe modifications, or more advanced treatments.
Book an appointment with our podiatrist at The Foot Practice to assess your condition.







