Ever looked down at your feet and seen discolouration, thickening or brittleness of your toenails? You might be one of the millions worldwide suffering from toenail fungus. Also known as onychomycosis, this common fungal nail infection affects about 10% of the population and up to 50% of people above 70. Despite its prevalence, many quietly suffer in silence, either too embarrassed to seek help or unaware that there are toenail fungus treatments available that can help them.
Toenail fungus is more than just an aesthetic issue. It’s a persistent infection that rarely resolves on its own if left untreated. What starts as a small white or yellow spot at the nail tip can gradually spread deeper and affect the entire nail. As the infection progresses, your nail will become more discoloured, thickened, brittle, and, in advanced cases, even odorous and painful.
Toenail fungus is a common challenge in Singapore’s warm, humid climate. The tropical environment creates an ideal breeding ground for fungi, so prevention and early treatment are especially important.

What Causes Toenail Fungus?
Toenail fungus occurs when fungi, usually dermatophytes, invade the nail through tiny cracks or separations between the nail plate and nail bed. Though dermatophytes are the most common culprits, yeasts and moulds can also be responsible. These opportunistic microorganisms thrive in warm, moist environments, which is exactly why feet, often confined in shoes where heat and sweat accumulate, are more prone to infection.
Several factors increase your risk of developing fungal nail infections. Most fungal nail infections are caused by fungi from athlete’s foot, which similarly thrives in warm, moist environments. Age also brings natural changes to nails, including slower growth, reduced blood circulation and more years of exposure to fungi.
Pre-existing conditions like diabetes, peripheral vascular disease, or immunosuppressive disorders increase your risk, as does frequent use of communal shower facilities, excessive sweating, damage to nails from sports, or ill-fitting shoes. Genetics can also play a role. Some people are naturally more prone to fungal infections than others.
The fungi that cause toenail infections are also contagious. They can spread from person to person through direct contact or via contaminated surfaces in swimming pools, changing rooms or shared personal items.

Types of Toenail Fungus: What You’re Dealing With in the Nail Bed
Not all toenail fungus infections are the same. Dermatophytes, a type of mould, are the primary cause of toenail fungal infections, also known as tinea unguium. Knowing what type affects your nails can lead to more targeted and effective treatment. These include:
- Distal subungual onychomycosis is the most common form, starting at the nail’s free edge and working towards the cuticle. The infection causes yellowing as it progresses beneath the nail, often leading to thickening and crumbling over time.
- White superficial onychomycosis typically presents as white spots on the nail surface that eventually cover the entire nail plate. Unlike other types, this infection remains superficial and doesn’t penetrate deep into the nail structure.
- Proximal subungual onychomycosis starts at the cuticle area and advances towards the nail tip – the opposite direction of distal subungual onychomycosis. This rarer form often indicates an underlying immunocompromised state, making it more concerning from a diagnostic perspective.
- Candidal onychomycosis affects fingernails more than toenails but can occur in individuals with chronic mucocutaneous candidiasis. This form often presents with significant inflammation around the nail fold and can cause the entire nail to thicken and separate from its bed.
- Total dystrophic onychomycosis is the most advanced stage, in which the entire nail unit is infected, thickened, and distorted. If left untreated for extended periods, this end-stage manifestation can result from any of the above types.

Symptoms and Effects of Toenail Fungus
Toenail fungal infections can manifest in many ways, affecting your nails’ appearance and health. Look out for:
- Discolouration: Affected nails may turn yellow, green, brown or black, deviating significantly from their natural colour.
- Thickening: The nail can become thicker and harder to trim or cut with regular nail clippers.
- Distortion: Infected nails can become misshapen or curved.
- Pain or Discomfort: You may experience pain or discomfort in the nail or surrounding skin, especially when applying pressure to the toe.
- Foul Odour: An infected nail and/or surrounding skin can emit a foul odour.
- Separation from the Nail Bed: The nail may lift away from the nail bed, causing increased pain and discomfort. This is a more severe symptom and should be addressed by a specialist.
- Crumbling or Brittleness: The nail can become brittle and break or split easily, necessitating professional treatment.

In severe cases, fungal nail infections can lead to:
- Increased Sensitivity or Pain: The nail and surrounding skin can become more sensitive and painful.
- Redness or Swelling: Inflammation around the nail can cause redness and swelling.
- Pus or Discharge: Pus or discharge from the nail or surrounding skin indicates a more serious infection within the toenail.
- Fever or Chills: These systemic symptoms mean the infection has become more severe and may require immediate medical attention.
You should recognise these symptoms early and treat them accordingly to prevent the infection from worsening and causing complications.
How Fast Does Toenail Fungus Spread?
The progression of toenail fungus varies from person to person, depending on the type of fungus, individual immune response, and environmental conditions. For many, the spread happens gradually. What starts as a small discoloured spot may take months to spread across the entire nail. However, this slow progression often lulls people into delaying toenail fungus treatment, allowing the infection to become more established.
Without treatment, the toenail fungus infection will spread in two ways, across the affected nail and potentially to adjacent nails. The fungus can colonise adjacent toenails by directly spreading under the skin or via contaminated socks, shoes, or personal grooming tools. In immunocompromised individuals or those with existing conditions like diabetes, the spread can be faster, sometimes affecting multiple nails within weeks rather than months.

The Limitations of Over-the-Counter Solutions
Many people try to treat nail fungus with over-the-counter products. While these toenail fungus treatments may work for mild, superficial infections, they often fail for more deep-rooted cases. Over-the-counter antifungal products struggle to penetrate the thick nail plate to reach the infection beneath. This limited penetration means that while surface symptoms may improve temporarily, the underlying fungal reservoir remains untouched, allowing the infection to persist and recur.
Consumer-grade treatments also require significant patience. Most manufacturers recommend using their products for 6 months or more, with visible improvement often not seen until several months into treatment. Many users stop treatment prematurely, believing the product is ineffective when, in reality, they have not used it long enough to see results.
For people with moderate to severe infections, relying on over-the-counter products only delays professional intervention, allowing the infection to become more established and potentially spread to other nails.

Light Therapy for Toenail Fungus
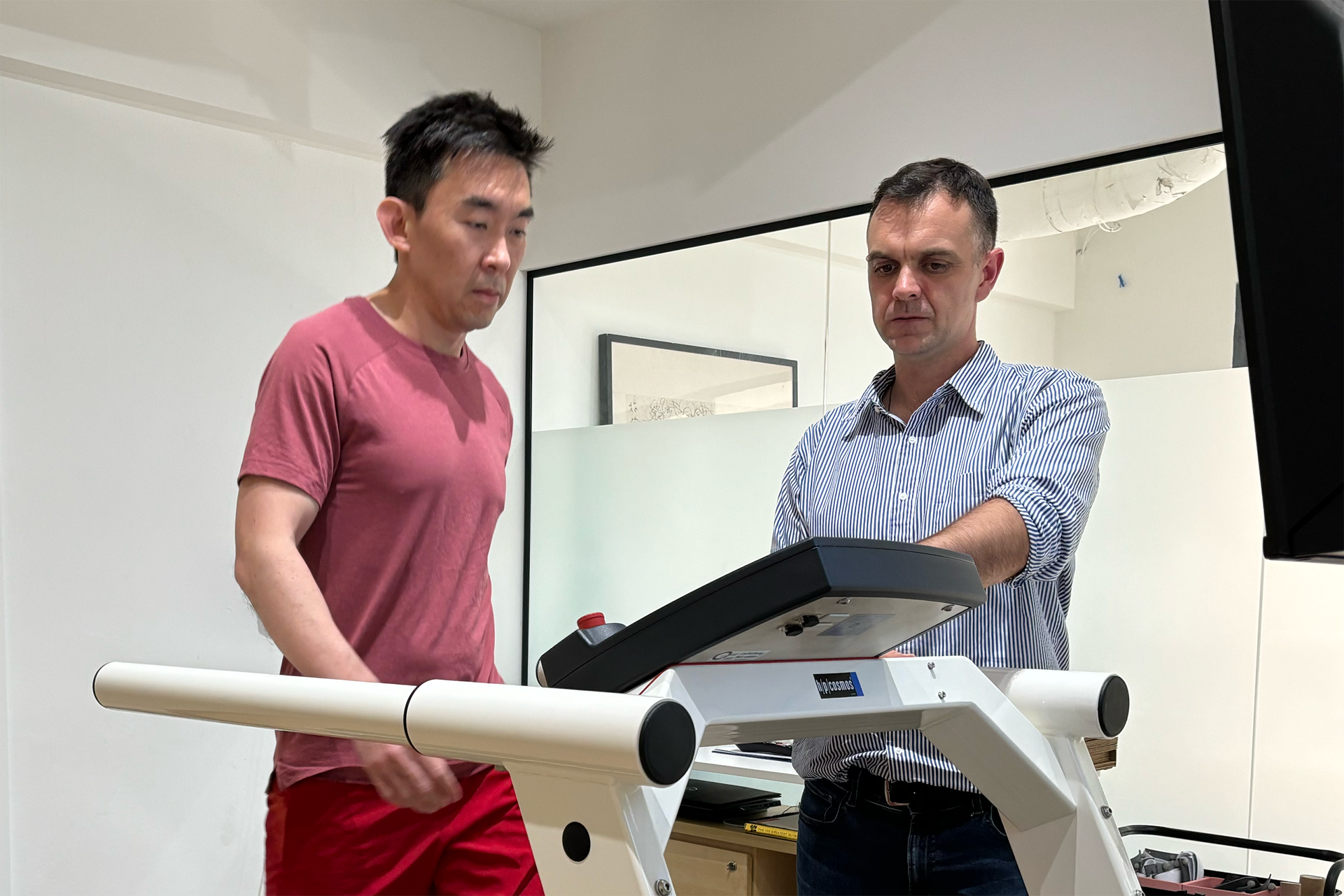
At The Foot Practice, we offer light-based care as part of a structured plan for managing toenail fungus. The ToeFX Therapy Light uses targeted LED wavelengths and is used in short, repeated sessions to support healthier-looking nails over time. It is a practical option for people who prefer a non-drug approach, or who want an extra layer of support alongside good nail and skin care.
It works best when matched to the correct diagnosis and nail type. Toenail fungus can sit under and within a thick nail plate, so results depend on how much of the nail is involved, how long it has been present, and whether the surrounding skin is affected.
We begin with an assessment to confirm it is a fungal nail infection, then build a comprehensive plan that may combine nail reduction and medical pedicures, topical care such as Suanfix where appropriate, footwear and hygiene guidance to reduce re-infection, and a paced schedule of ToeFX light sessions, all aimed at improving comfort, nail appearance, and recurrence control.

Suanfix Antifungal Cream for Toenail Fungal Infections
The Foot Practice offers patients a safe, natural, and highly effective topical treatment for toenail fungus. A natural cure for fungal nail infections, our unique treatment solution involves Spirulina, a dried form of a natural bacteria with fungicidal properties, that kills nail fungus instantly and permanently. The solution also uses the same natural antifungal properties to repair damaged nails by regenerating the infected nail bed.
This breakthrough in toenail fungus treatment in Singapore combines traditional knowledge with modern science. Unlike conventional treatments that often contain harsh chemicals, The Foot Practice’s Spirulina-based formula has potent antifungal action without harming the nail. Our patients often appreciate that this effective approach uses natural ingredients.
Beyond Treatment to Prevent Fungal Nail Infections
Professional podiatric care goes beyond managing the infection. It includes preventative and personalised advice tailored to each patient’s risk factors. Keeping feet dry and cool is key to preventing fungal nail infections, especially in warm and humid environments. For people with diabetes or circulatory issues, this preventative aspect is even more important, as minor foot problems can become serious complications.
The Foot Practice’s expert podiatrists provide personalised advice on shoe selection, recommending shoes that allow good ventilation and minimal moisture. They counsel patients on proper foot hygiene practices, including drying between toes after bathing and sanitising footwear.
Our podiatrists may recommend regular follow-up visits for those with recurring infections to monitor nail health and address any early signs of reinfection before it becomes established. These small tips can make a world of difference in preventing another pesky toenail fungus infection.

Complications and Related Health Conditions
If left untreated, fungal nail infections can lead to various complications and related health conditions, some of which can be serious. These include:
- Cellulitis: A bacterial infection of the skin and underlying tissues that can develop if the fungal infection spreads beyond the toenail.
- Abscesses: Painful, pus-filled pockets that can form in the nail or surrounding skin, requiring medical attention.
- Osteomyelitis: A bone infection that can occur if the fungal infection spreads to the bone, requiring more aggressive treatment.
- Sepsis: A life-threatening condition that occurs when the infection enters the bloodstream and causes widespread inflammation and organ failure.
- Diabetic Foot Ulcers: People with diabetes are at higher risk of developing foot ulcers, and fungal nail infections can exacerbate them.
- Nail Loss: Severe or untreated fungal infections can lead to the complete loss of the affected nail.
When to See a Professional
While mild cases of toenail fungus may respond to home treatment, certain situations require prompt professional evaluation. If you’re experiencing pain in the infected nail, notice the fungus spreading to multiple toenails, or have underlying conditions such as diabetes, peripheral vascular disease, or immunosuppression, professional podiatric care is essential.
Similarly, if you’ve tried over-the-counter treatments for several months without improvement, contact The Foot Practice to explore how our naturally derived solution for toenail fungus can help your feet heal.