The Hidden Pain Behind Posterior Shin Splints
When that dull ache starts to creep along the inner back of your lower leg, most experienced runners and athletes know the diagnosis before they even see a doctor: posterior shin splints. This frustrating condition – medically known as posterior tibial stress syndrome – can turn an enthusiastic training schedule into weeks of rehab and frustration.
Posterior shin splints are one of the most common lower limb injuries among active individuals. They affect as many as 35% of runners at some point in their athletic careers, who feel pain along the inner back of their lower leg. Fortunately, various intervention strategies are available to help alleviate your discomfort and get you back on track.

What Are Shin Splints?
Shin splints, medically known as medial tibial stress syndrome, are a common overuse injury that affects many athletes and active individuals. This condition occurs when the muscles, tendons, and bone tissue around the shinbone (tibia) are subjected to excessive stress.
Unlike their anterior counterparts that affect the front of the shin, posterior shin splints cause pain and inflammation along the inner posterior border of the tibia, where several important muscles attach to the bone. These muscles – primarily the posterior tibialis – become overworked or irritated, causing microtears in the connection between the muscle and bone, inflammation of the periosteum (the outer layer of bone), or, in more severe cases, stress reactions within the bone itself.
Unlike a stress fracture (which posterior shin splints can progress into if neglected), the discomfort often eases up once muscles warm up and then returns with more intensity as activity continues, potentially leading to severe pain. This sneaky pattern leads many to ‘push through’ the pain, a move that only worsens the condition and extends recovery time.

Symptoms of Posterior Shin Splints
The most common symptom of posterior shin splints is pain along the inner back edge of the shinbone. This pain can range from a dull ache to sharp, localised pain, making it a major obstacle to physical activity. Other symptoms include mild swelling, tenderness and stiffness in the lower leg. The pain gets worse with physical activity and can even persist during rest if not appropriately addressed. Early recognition of these symptoms is key to timely intervention and treatment.

Causes and Risk Factors
Posterior shin splints are often the result of overuse or repetitive stress on the lower leg muscles and bones. Several risk factors can increase the likelihood of developing this condition:
- High-Impact Activities: Engaging in activities like running, jumping or dancing that put repeated stress on the lower legs.
- Sudden Increases in Activity: Rapidly increasing physical activity or changing an exercise routine without proper preparation.
- Poor Footwear: Wearing shoes that lack proper support or cushioning increases stress on the lower legs.
- Biomechanical Issues: Conditions like flat feet or overpronation that alter the natural mechanics of the foot and leg.
- Insufficient Stretching or Strengthening: Failing to stretch or strengthen the lower leg muscles can lead to imbalances and increased stress on the tibia.
By knowing these causes and risk factors, individuals can take proactive steps to prevent shin splints and reduce the risk of persistent pain and inflammation in the lower legs. Proper training techniques, supportive footwear and stretching and strengthening exercises effectively reduce the risk of shin splints.

How Podiatry Helps Beyond Rest
While helpful, the traditional posterior shin splint treatment approach – rest, ice, compression and elevation – is just the starting point for proper management at home. A podiatrist offers a more nuanced and effective approach to recovery and preventing recurrence. This process begins with a complete physical examination to diagnose posterior shin splints and identify underlying biomechanical issues.
“Posterior shin splints recovery involves addressing the root biomechanical causes, not just managing symptoms”,’ says leading sports podiatrist Tim Maiden at The Foot Practice. “That’s why comprehensive assessment is the foundation of effective treatment.”
The podiatric approach begins with a biomechanical evaluation, carefully examining gait patterns, foot posture, and muscular function. Special attention is given to overpronation, an excessive inward rolling of the foot during the gait cycle, which places significant stress on the posterior tibialis muscle and is implicated in most posterior shin splint cases.
This holistic assessment identifies the unique combination of factors contributing to each patient’s condition, allowing for highly individualised treatment protocols often involving a physical therapist for tailored rehabilitation exercises.

Benefits of Gait Analysis
One of the most significant developments in podiatric care is the RehaWalk® pressure sensor treadmill, which provides unparalleled insight into the forces at play during movement.
The RehaWalk system allows our podiatrist at The Foot Practice to measure exactly what’s happening during the gait cycle rather than making educated guesses. We can develop interventions based on objective measurements rather than generalised posterior shin splint treatment protocols.
In addition to the RehaWalk system, magnetic resonance imaging (MRI) can be used to visualise small cracks in the tibia and other anatomical conditions that may contribute to shin splints. This advanced system captures thousands of data points per second as patients walk or run, creating detailed visualisations of pressure distribution, timing imbalances, and biomechanical irregularities that standard visual assessments might miss. Your podiatrist can analyse this in-depth data to form a thorough understanding of exactly how and when excessive forces are transmitted through the affected structures in your leg.
This precision extends to monitoring progress throughout the rehabilitation process. As recovery progresses, follow-up assessments of the RehaWalk system show improvements in pressure distribution and biomechanical efficiency, providing tangible evidence of recovery. This can go a long way towards restoring your confidence and reinforcing positive lifestyle changes.

Supportive Footwear
Many affected individuals are unaware that their trainers contribute to their condition. Shoes that provide enough support and cushioning to prevent excessive stress on the lower legs are recommended.
For posterior shin splints, shoes that require more activation of the posterior tibialis muscle, especially worn or unsupportive shoes that don’t control excessive pronation, often worsen symptoms. Similarly, transitioning to minimalist shoes without proper conditioning can often trigger episodes of posterior shin splints in enthusiastic but unprepared runners.
Podiatric footwear assessments examine not just shoe type but specific structural characteristics and how they relate to individual biomechanics. Factors such as midsole density, heel counter stability, torsional rigidity, and wear patterns all contribute to foot health and influence gait mechanics.
Based on assessment findings, podiatrists may recommend modifications to existing shoes or purchase entirely new shoes with medial support structures, appropriate cushioning profiles, and biomechanically correct heel-to-toe drops. These recommendations are tailored to individual needs, not generic prescriptions for any foot.

Mobilisation to Restore Function
While rest is important in the early stages of posterior shin splint recovery, prolonged inactivity can hinder healing by allowing supporting tissues to weaken and adaptive patterns to develop. Progressive mobilisation exercises, when carefully introduced and monitored by podiatrists, maintain tissue mobility while promoting healing.
These controlled movements begin with non-weight-bearing ankle circles and toe curls, stimulating circulation without stressing damaged tissues. As healing progresses, exercises gradually add partial weight-bearing activities and controlled strengthening of the posterior compartment muscles.
Specific posterior shin splint stretches and strengthening exercises targeting the posterior tibialis muscle are particularly effective. These include seated towel stretches and standing wall exercises that gently lengthen tight tissues without irritating inflamed areas. Unlike generic calf stretches that many patients attempt on their own, properly instructed podiatric stretching protocols ensure precise targeting and a gradual increase, ensuring stable recovery without overloading the muscles.

Customised Support of Orthoses
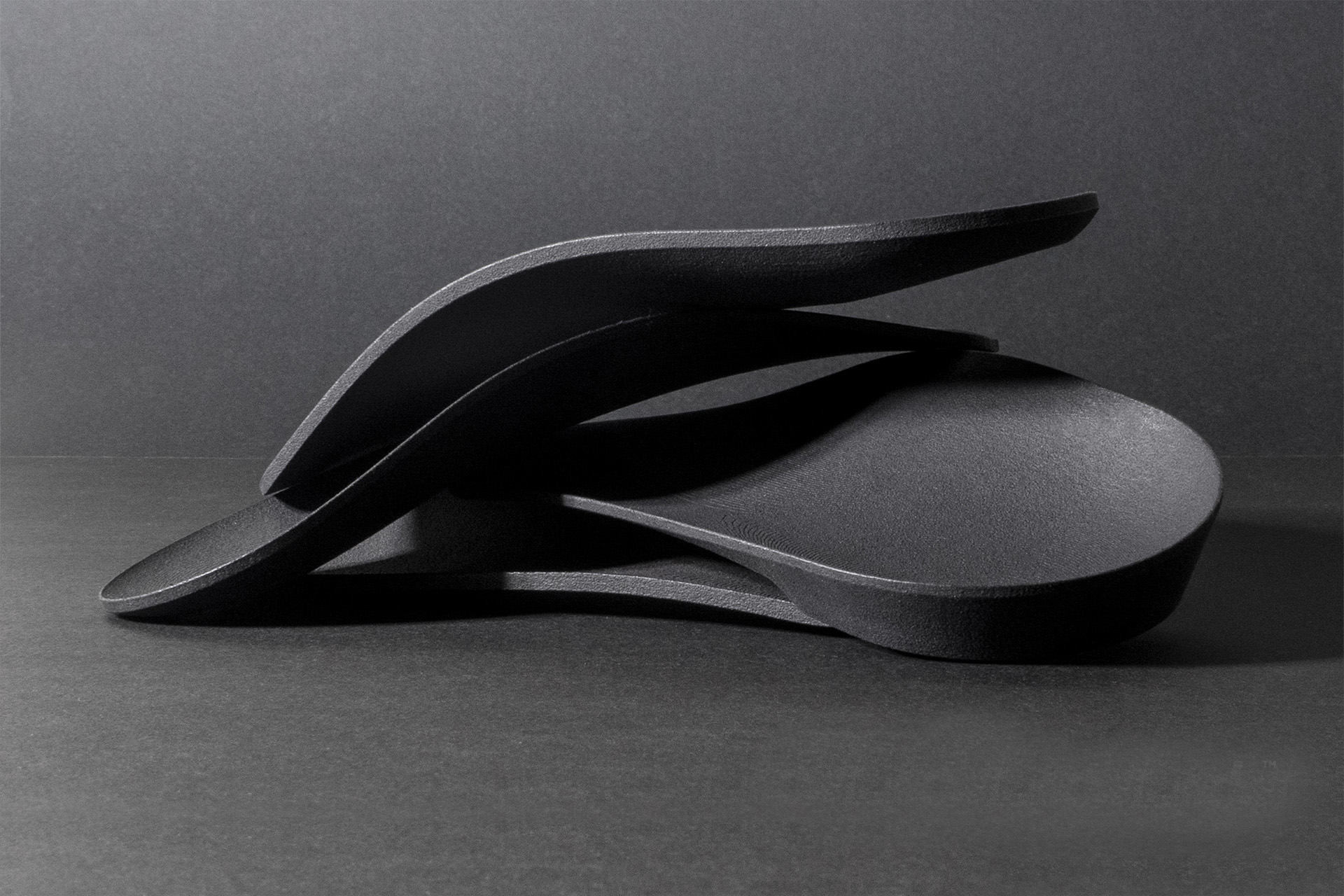
Custom orthotic devices and shoe inserts are essential during the healing and return-to-activity phases for many patients, especially those with structural foot abnormalities or persistent biomechanical inefficiencies. Unlike off-the-shelf inserts, podiatric orthoses are precision-crafted, utilising data from a detailed assessment of an individual’s foot structure and function.
Orthotic fabrication at The Foot Practice uses advanced computer modelling and pressure data from systems like RehaWalk® to 3D print your custom orthoses. This integration enables devices to address the specific biomechanical factors contributing to each patient’s posterior shin splints, rather than applying generic corrections that may not effectively target the issue.
For posterior tibial stress syndrome, orthoses typically include medial arch support to reduce pronation forces, stabilising posts to control calcaneal (heel) position, and sometimes specific accommodations for anatomical variations, such as forefoot varus. These elements work together to redistribute pressure away from stressed tissues while supporting proper functional movement patterns.
Breaking Down Scar Tissue with Shockwave Therapy
Extracorporeal Shockwave Therapy is particularly effective for managing posterior shin splints that do not respond to conventional approaches, especially in cases with significant scar tissue development or chronic inflammation. This non-invasive treatment delivers precisely targeted acoustic pulses that penetrate deeply into affected tissues, stimulating healing responses without surgery.
The controlled microtrauma created by Shockwave Therapy increases blood flow, releases growth factors and breaks down pathological scar tissue that can cause posterior shin splint symptoms to linger long after initial inflammation has subsided. Multiple studies show significant pain reduction and functional improvement after Shockwave Therapy sessions, often after just 3-5 treatments.

Integrated Approach to the Management of Posterior Shin Splints
The best podiatric management of posterior shin splints combines advanced interventions with traditional therapies, using individual assessment findings. A patient with significant biomechanical abnormalities might start with orthotic therapy and footwear modifications and then add mobilisation exercises as pain decreases. Another with chronic tissue changes might begin with Shockwave Therapy and specific posterior shin splints taping techniques, and then transition to functional rehabilitation.
Throughout this process, the RehaWalk system provides objective measurements of progress, allowing treatment protocols to be adjusted based on measurable improvements, rather than relying solely on subjective reporting. This data-driven approach means that interventions evolve as healing progresses through the different stages.
This podiatric framework addresses the multiple factors contributing to posterior shin splints, enabling patients to achieve symptom relief and correct the underlying cause of their condition. This can make the difference between a temporary fix and long-term recovery.
For those suffering from this condition, contact The Foot Practice today for an initial consultation for your posterior shin splints.






