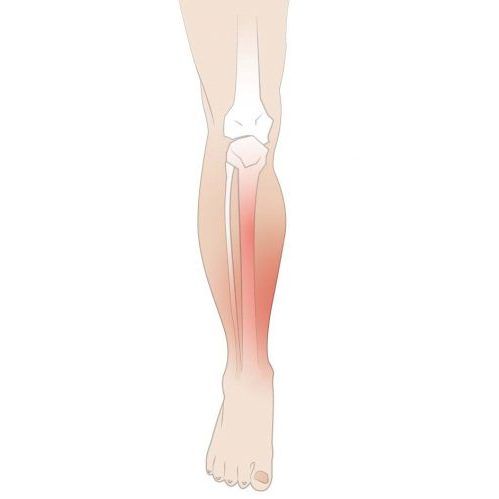
When your shins start to ache after that new training program you’ve been working on, you’re experiencing one of the most common yet annoying injuries athletes face. Medically known as medial tibial stress syndrome, shin splints are a common exercise-related problem characterised by pain along the inner edge of the shinbone.
Shin splints can occur when individuals suddenly increase their training intensity or duration. They’re more than just a temporary setback. They’re a sign of an imbalance that needs attention. While rest and ice packs are good first steps, modern podiatric approaches offer a more holistic way to recover and prevent future episodes of shin splints.
What Are Shin Splints: Causes of Shin Pain
Shin splints develop when athletes increase their training too quickly or change their routine without proper adaptation. The condition is typically caused by excess stress on the lower leg’s tendons, muscles and bones, particularly along the inner border of the tibia, the shinbone. This overwork causes inflammation, micro-tears in the tissues that connect muscle to bone, and sometimes even stress reactions in the bone itself.
The classic presentation is aching and tenderness along the inner aspect of the shin, sometimes with mild swelling. Initially, the pain may subside once you warm up, but as the condition progresses, the pain may persist throughout your activity and, eventually, even at rest. Both legs can be affected, but it’s not uncommon to have shin splints on one side, often reflecting biomechanical imbalances or training patterns. It is essential to take several weeks of rest for proper recovery. Untreated shin splints can lead to a stress fracture, characterised by small cracks in the tibia due to stress and overuse.
While many cases respond to home remedies like ice, rest and anti-inflammatory medications like ibuprofen, persistent or recurring shin splints need professional attention. This is where comprehensive podiatric care comes in – not just treating symptoms but addressing the underlying causes holistically.

Shin Splints Symptoms
Shin splints are characterised by pain and discomfort along the inner edge of the shin bone. The pain can vary in nature, being sharp, dull, or aching, and often worsens with physical activity. Common symptoms of shin splints include:
- Pain along the inner edge of the shin bone
- Mild swelling in the lower leg
- Tenderness to the touch
- Pain that intensifies with physical activity
- Pain that persists even during rest
In severe cases, shin splints can lead to more serious complications, such as stress fractures or chronic exertional compartment syndrome. If you experience persistent pain or swelling in your lower legs, it is crucial to seek medical attention, as early intervention can prevent these complications and promote a quicker recovery.

Who Is At Risk of Shin Splints
People who are more at risk of getting shin splints are:
- Athletes who play sports on a hard surface and stop and start suddenly during the game.
- Runners who have just started running or have just increased their training program.
- People who have to march for many hours.
- Cross-country runners or those who run or walk on uneven terrain.
- People have high arches or flat feet.
- Military recruits due to the intensity and changes in physical training routines.
Wearing proper-fitting athletic shoes is crucial to preventing shin splints. Good cushioning and support tailored to your foot shape and specific sport can make a significant difference.

How Are Shin Splints Diagnosed?
Diagnosing shin splints typically involves a combination of physical examination, medical history and imaging tests. Our podiatrists at The Foot Practice will assess your lower leg for tenderness, swelling and pain during a physical exam. They will also inquire about your exercise routine, medical history and any previous injuries to comprehensively understand your condition.
Imaging tests, such as X-rays or bone scans, may be ordered to rule out other conditions like stress fractures or tendinitis. Sometimes, you may be referred to a physical therapist or orthopaedic surgeon for further evaluation and shin splint treatment.

How Podiatry Helps With Shin Splint Recovery
The foundation of recovering from shin splints starts with a thorough assessment. The Foot Practice’s podiatrists use advanced diagnostic tools beyond the physical examination to see how your feet and legs move.
One of the advantages of coming to our leading podiatry clinic is the holistic approach to care. Instead of just relieving pain, our podiatrists investigate the biomechanical causes of the condition.
Advanced tools like the RehaWalk® pressure sensor treadmill give The Foot Practice an edge in diagnosing subtle movement patterns. This state-of-the-art system captures thousands of data points while a patient walks or runs and provides real-time pressure distribution, stride dynamics and foot placement analysis. Identifying irregularities such as overpronation or asymmetrical loading helps podiatrists design precise interventions to reduce tibial stress and support long-term recovery.
In many cases, biomechanical imbalances can be addressed with custom orthoses. These are insoles specifically designed to support the foot’s natural alignment, distribute force evenly, and reduce repetitive strain. Well-crafted orthoses are especially effective in people with flat feet or high arches to prevent overloading of the tibial region. Many athletes also use insoles to prevent shin splints as a long-term strategy.
Proper footwear is another important consideration. Footwear assessments by a podiatrist take into account not just shoe design but how a person moves in their shoes. Worn-out trainers and shoes with insufficient arch support or inappropriate types for a given activity can all worsen or trigger shin pain. Podiatrists recommend styles based on individual needs and can also advise on modifications or replacement intervals.
Rehabilitative support often includes mobilisation exercises which target flexibility and strength in the lower leg. Tight calves or weak foot muscles can contribute to abnormal loading and inefficient movement. Customised exercises help recondition the muscles and improve range of motion and balance. These physical interventions are key to recovering from shin splints, rebuilding resilience and reducing re-injury risk.
In more stubborn cases, Shockwave Therapy may be recommended. This noninvasive treatment delivers targeted acoustic waves to the affected tissue, stimulating blood flow, accelerating tissue repair and reducing inflammation. It has been particularly helpful for persistent or recurring shin pain that hasn’t responded to conventional methods. Combined with other podiatric strategies, it can significantly shorten shin splint recovery time.

Insoles To Prevent Shin Splints
While generic insoles promise to prevent shin splints, custom orthoses prescribed by podiatrists deliver much more specific support. Using data gathered from dynamic assessment, practitioners design orthotic devices that modify specific problematic movement patterns rather than just adding cushioning.
For those with excessive pronation (flat feet), orthoses provide medial support that reduces internal rotation stresses on the tibia. For those with high arches, orthoses offer greater shock absorption to compensate for naturally reduced flexibility. Most importantly, these interventions synergise with properly fitted footwear to create a comprehensive support system. Wearing supportive shoes with good cushioning is crucial as part of a comprehensive management plan to reduce stress on the shins during daily activities.
Modern orthotic fabrication has come a long way, with materials ranging from semi-rigid polypropylene to composite carbon fibre allowing precise motion modification without excess bulk. The newest generations of orthoses can be remarkably thin yet effective, fitting into athletic and everyday footwear.

Beyond Recovery towards Prevention
Most importantly, comprehensive podiatric care goes beyond symptom resolution to long-term prevention. These interventions change how forces are distributed through the lower limb during activity by addressing underlying biomechanical factors. Avoiding putting too much stress on the muscles, tendons, and bones of the lower leg is crucial to preventing injuries like shin splints and stress fractures.
Podiatrists guide progressive loading strategies for athletes returning to training that respect tissue adaptation timeframes. This may include recommendations about surfaces (gradually transitioning from softer to harder running surfaces), footwear rotation (alternating between models to vary stress patterns), and training periodisation (strategically varying intensity and volume). Running on hard or uneven surfaces can exacerbate the risk of developing shin splints, so incorporating varied training surfaces is essential.
Many practitioners also include regular monitoring in prevention programmes, scheduling periodic check-ins to assess orthotic function, footwear condition and movement quality before symptoms recur. This proactive approach is particularly useful for competitive athletes and those with anatomical predispositions to shin splints.
Get Help with Your Shin Splints
With proper care, most people can fully recover from shin splints. It’s not just about the symptoms but also about the functional and structural causes. Get in touch with The Foot Practice today if you have shin splints!







