For people with diabetes, foot health is not just about comfort, it’s about preventing serious complications, especially for early-stage diabetic foot ulcers. These ulcers can start as small, seemingly minor injuries and if left unchecked, they can quickly become infections, present mobility issues and even amputation in extreme cases. Early management makes all the difference. That’s where podiatry comes in.
Podiatry offers targeted interventions to address the specific challenges of diabetic foot conditions. From prevention to advanced diagnostics, podiatry ensures patients get the necessary care, minimising risks and maximising foot health.
How Early Stage Diabetic Foot Ulcers Happen
Ulcers develop when minor injuries such as cuts, blisters or pressure sores don’t heal properly due to the physiological changes caused by diabetes. High blood sugar levels affect the body’s immune system, specifically white blood cells. This means the body can’t repair tissues.
Diabetes also causes neuropathy, which reduces sensation in the feet. People with diabetes often don’t feel their feet are injured as they don’t have feeling in their extremities. They don’t feel pain and thus don’t detect injuries early. Minor wounds are subjected to continuous pressure or friction without the pain response and worsen over time.
Poor circulation, another common complication of diabetes, further hinders healing by reducing blood flow to the extremities so the essential nutrients can’t reach the affected area. This creates an environment where minor wounds can quickly become early-stage diabetic foot ulcers. Infections can set in quickly due to a weakened immune response, complicate recovery and increase the risk of serious complications.
These show why early podiatric intervention is key to preventing and managing diabetes-related foot complications, including ulcers.

What is a Diabetic Foot Ulcer?
A diabetic foot ulcer is a serious complication of diabetes where a wound or sore on the foot doesn’t heal. Affecting 15% of diabetics, if left untreated, this can lead to severe complications, including amputation.
Diabetic foot ulcers are a combination of complications from high blood sugar levels, diabetic neuropathy and poor circulation. High blood sugar levels impair the body’s ability to heal. Diabetic neuropathy reduces sensation in the feet so people with diabetes don’t feel their feet are injured. Poor circulation complicates healing by reducing blood flow to the affected area. Understanding these factors is key to early detection and treatment of diabetic foot ulcers.

Causes and Risk Factors
Diabetic foot ulcers are caused by a combination of factors that often work together to create a perfect storm for foot complications. Chronically high blood sugar levels can damage nerves and small blood vessels, reduce blood flow and increase the risk of foot ulcers.
Diabetic neuropathy, a common complication of diabetes, causes nerve damage, which causes numbness, tingling and loss of sensation in the feet. This makes it challenging to detect foot injuries or complications early.
Poor circulation, another common issue in diabetic patients, hinders healing by reducing the blood flow needed for tissue repair — foot injuries, whether from trauma or ill-fitting shoes, can increase the risk of foot ulcers. Poor foot care practices, such as not treating sores and cuts with basic first aid, can also increase the risk of foot complications. Knowing these risk factors is key to preventing and managing diabetic foot ulcers.

Symptoms and Signs
Knowing the symptoms and signs of diabetic foot ulcers is key to early intervention and treatment. Common symptoms are numbness or tingling in the feet, pain or burning sensation, and weakness or fatigue in the feet. Difficulty walking or standing can also indicate a developing foot ulcer. Visible signs are foot ulcers or sores that don’t heal, skin colour or temperature changes, and redness or swelling around the affected area. In severe cases, there may be pus or discharge from the wound and foul odour.
Knowing these symptoms and signs can help you seek medical attention early and prevent further complications.
Stages of Foot Ulcers
Diabetic foot ulcers can progress through several stages, each requiring a different level of care and intervention:
- Stage 1 The foot may look normal with no visible changes, but underlying issues like reduced blood flow or nerve damage are already present.
- Stage 2 There is a noticeable loss of blood flow or nerve damage, making the foot more prone to ulcers.
- Stage 3 By this stage, pressure on the affected area should be avoided to prevent further damage.
- Stage 4 This requires hospitalisation and surgical intervention to manage the ulcer and prevent severe complications.
- Stage 5 Dead skin and tissue may develop, and the limb may require amputation to prevent life-threatening complications from developing.
Knowing these stages helps you understand the severity of the condition and the importance of early treatment of diabetic foot ulcers.
Complications of Diabetic Foot Ulcers
If left untreated, diabetic foot ulcers can lead to severe complications that can affect a patient’s quality of life. One of the most common complications is an infection, where bacteria enter the wound and can spread to the bones, or sepsis, a life-threatening condition.
Gangrene, where dead skin and tissue develop, often requires amputation to prevent further harm and prevent life-threatening complications.
Diabetic foot ulcers can also cause mobility issues, making it hard to do basic daily activities like walking. The pain, discomfort and emotional distress can significantly reduce the quality of life. Early detection and proper management are key to preventing these severe complications and ensuring well-being.

Diabetic Foot Screenings
Diabetic foot screenings are the key to ulcer prevention and management. Regular screenings help identify early signs of diabetic foot ulcers, like skin discolouration and swelling, which is key to early intervention. Screenings from a trained professional involve thoroughly examining the feet to identify risk factors like poor circulation, nerve damage or deformities. Early detection of these allows for early intervention and prevents minor wounds from becoming early-stage diabetic foot ulcers.
During a screening, a podiatrist will assess skin integrity, check for pressure points, and test for neuropathy using tools like monofilament testing. The latter is important so you and your podiatrist can know how sensitive your feet are and which areas to watch out for. This proactive approach helps identify problem areas before they become a problem and allows patients to take preventive measures to protect their feet.

Footwear Assessments: Preventing Pressure and Injury
For people at risk of developing diabetic ulcers, proper footwear is more than a comfort issue — it’s a necessity. If you’re unsure what type of footwear you should be wearing or if the footwear you have now is sufficient, a footwear assessment from a podiatrist is key. In these assessments, a podiatrist will ensure patients wear shoes that provide adequate support, reduce pressure on vulnerable areas and minimise the risk of injury.
A footwear assessment is an investment in long-term foot health.
Mobilisation Exercises: Circulation and Strength
Good circulation and muscle strength in the feet are crucial for people with diabetes. Mobilisation exercises prescribed by a podiatrist can improve blood flow, increase flexibility and strengthen the muscles that support the foot, which helps manage existing early-stage diabetic foot ulcers and prevent new diabetic ulcers from forming.
Simple activities like toe curls, ankle rotations and stretching can also be part of a daily routine to keep the feet healthy. Podiatrists will guide you on proper techniques and tailor exercises to your needs to get maximum benefit without strain.
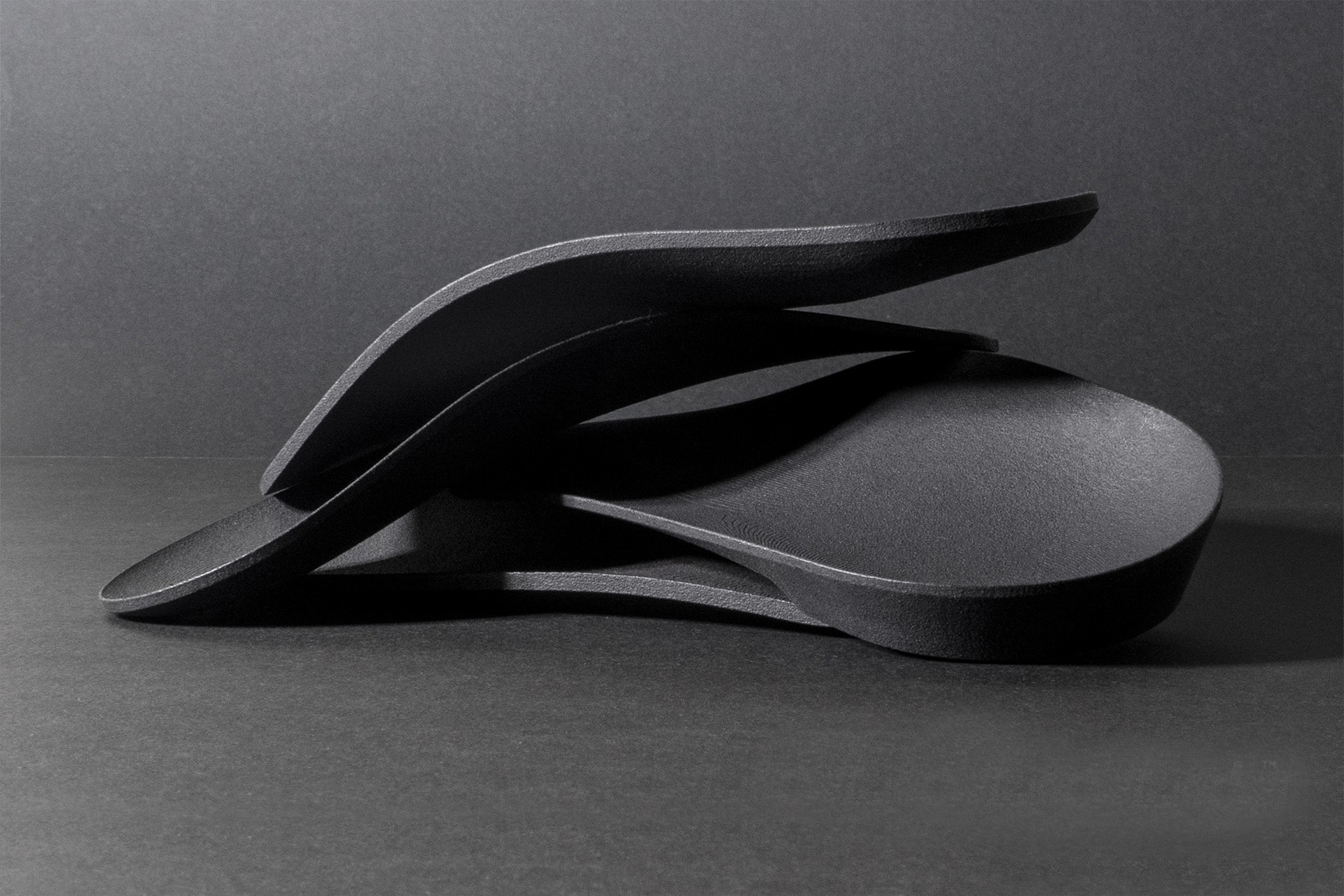
Orthoses Support and Protect the Foot in Diabetic Neuropathy
Orthotic devices are essential in managing diabetic foot conditions, especially in early-stage diabetic ulcers. These custom-made devices provide optimal support, correct biomechanical issues, and reduce pressure on vulnerable foot areas. This can help prevent ulcers or manage existing ones, especially when your podiatrist knows which areas of your foot are prone to friction and pressure.
For example, orthoses can offload pressure from a developing ulcer, giving the affected area time to heal without further irritation. Podiatrists use advanced techniques to design functional and comfortable orthoses so patients can wear them daily.
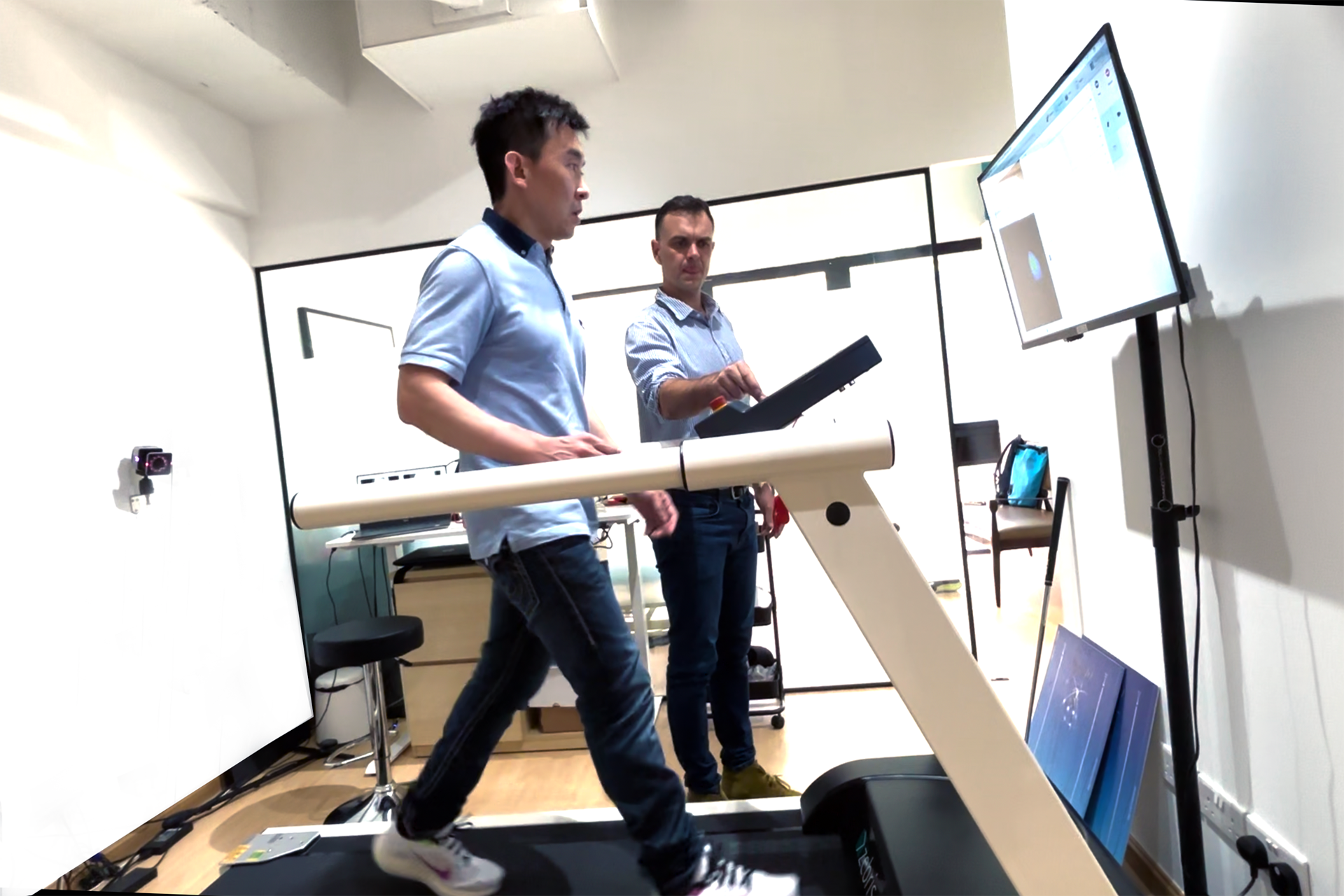
RehaWalk Gait Analysis Changes Diabetic Foot Care
One of the most advanced tools in diabetic foot management is the RehaWalk® pressure sensor gait analysis system. This technology provides a detailed map of how pressure is distributed across the foot during movement, showing areas of concern that may not be visible to the naked eye, especially in patients with diabetic ulcers.
By analysing gait patterns, RehaWalk® helps podiatrists identify biomechanical issues and develop targeted management strategies. For patients with early-stage diabetic foot ulcers, interventions can be tailored to their specific needs, whether adjusting footwear, modifying orthoses or recommending specific exercises. The ability to monitor progress over time through several sessions also ensures interventions remain effective as the condition changes.
Why Podiatry is Good for Early-Stage Diabetic Foot Ulcers
The holistic approach of podiatry makes it a valuable resource for managing diabetes-related foot complications, including early-stage diabetic foot ulcers. By addressing the symptoms and the underlying causes of early-stage diabetic foot ulcers, podiatrists give patients control over their foot health.
- Prevention: Through screenings, footwear assessments, and education, podiatry reduces the risk of ulcers developing in the first place.
- Early Intervention: Advanced diagnostic tools and individualised management plans mean ulcers are managed before progressing to more serious stages.
- Holistic Care: Podiatry offers various interventions to support overall foot health, from orthoses to mobilisation exercises.
- Better Outcomes: With RehaWalk, podiatrists can deliver precise care, faster healing and fewer complications.
Early-stage diabetic foot ulcers don’t have to lead to more complications. You can manage this condition effectively and live well with timely intervention and expert care. Podiatry offers a comprehensive approach to diabetic foot care, combining prevention, technology and individualised treatment to address the specific needs of diabetic patients. Contact The Foot Practice today to schedule an appointment if you suspect you have an early-stage diabetic foot ulcer.





